Introduction
In the polyphasic sleep community, selective sleep deprivation is an overall unfamiliar concept. In fact, this term oftentimes appears confusing and misleading with the generic sleep deprivation. However, on a polyphasic sleep schedule, it is actually a very common phenomenon. In addition, the focus of this post is to shed light on:
- How exclusive SWS deprivation symptoms are different from REM equivalents.
- Explain how certain polyphasic schedules are more difficult to adapt than others, despite similar total sleep.
Regardless, do note that there is a scarcity of information on selective sleep deprivation mechanics. Furthermore, sleep deprivation studies never last long. Therefore, we can only extrapolate the information and conclusions from short-term reduced or experimental monophasic sleep studies.
Content
- Generic sleep deprivation vs selective sleep deprivation
- Selective SWS deprivation
- Selective REM deprivation
- Implications on polyphasic sleep schedules
Generic Sleep Deprivation vs Selective Sleep Deprivation
We have heard a lot about how sleep deprivation overall negatively corrodes health. While that is true, it often implies deprivation of either REM sleep or SWS sleep, or both stages. It is, in short, an umbrella term for reduction in duration of these vital sleep stages. Poor quality sleep yields diverse results in sleep EEG. Without sufficient sleep hygiene practice, sleeping a full 8-9-hour core sleep can still be as tiresome as ever. Thus, sleep duration is not the sole determinant for human well-being.
On the other hand, selective sleep deprivation is the curtailment of either REM or SWS. Note that, interestingly enough, there has never been any mention on selective light sleep deprivation. Because both vital sleep stages play different roles, it is reasonable to expect specific curtailment effects from sleep deprivation.
Note:
- It is impossible to exactly know if you are missing out on some SWS or REM without a reliable sleep tracker. Refer to sleep tracking for more information.
- Regardless of your current sleep pattern, periodically having a health check is a good idea. This way your physicians and doctors can know if you need to improve your sleep.
Selective SWS Deprivation
Sleep Architecture
Under this selective sleep deprivation condition, researchers use auditory stimuli to disrupt SWS and minimize its duration1,2. Specifically, total sleep duration and REM duration remain unchanged. The only changes in sleep architecture are:
- The hefty decrease in SWS duration,
- A massive increase in NREM2 duration. This is because said auditory stimuli eliminate delta waves of SWS on an EEG. Despite the fact that sleepers remain asleep, their brainwaves now change and they shift back to light sleep. Auditory stimuli, however, need to be weak enough to keep subjects asleep.
Even though subjects sleep a whole night, they remain sleep deprived. The only saving graces are the benefits from a sufficient REM duration and some NREM2. This concept, again, largely mirrors how sleeping through the night does not always guarantee enough vital sleep stages. As a result, it is necessary for even polyphasic sleepers to sleep in a completely quiet environment at night.
Overall, under normal sleep conditions and good sleep hygiene practice, a sufficiently long core sleep will cover all SWS requirement. Because of the usual extremity of the SWS deprivation experiments, it is often difficult to completely miss all SWS in a normal core sleep.
Effects on Health
Below are certain symptoms of SWS deprivation. Nevertheless, this list does not contain absolute information. Certain studies only have female subjects, or only partially deprive SWS in subjects, for example. Some of these effects may be precursors or similar to the long-term effects in SWS reduction.
As such, this list only details mostly short-term symptoms that polyphasic sleepers also possibly run into.
- Decreased pain threshold, increased fatigue, discomfort and inflammatory flare response in skin1. However, these results were from middle-aged women only.
- Fibromyalgia formation1
- Weakened attention resources and error detection2
- Deficits in attention system that are exacerbated in insomniac individuals3
- Impaired explicit/declarative memories for visuospatial information and explicit verbal episodic memories4
- Overall decreased pain threshold and sufficient SWS during recovery sleep reversed the effect5
- Lowered morning testosterone production and deficits of androgens (steroid hormones)6
- Less sleep inertia generation, which bluffs the misconception of good sleep. Despite the good news, during the wake periods afterwards, there is a clear impairment in cognitive performance accuracy7.
- More vigilance lapses, decreased hippocampus activation on encoding memories8.
- Biomarker for schizophrenia9
- Changed melatonin secretion and glucose tolerance10
- Adolescents without high metabolic reserves face decreased insulin sensitivity11.
- Blood pressure dipping during nocturnal sleep, but mostly in the earlier sleep cycles12.
Cautions for Polyphasic Sleepers
The following interpretations are from the aforementioned studies. Therefore, it is necessary to account for individual variability.
- Attenuated attention resources imply that it will be difficult to physically stay awake. This also means adapting polyphasic sleepers will run into microsleeping more often. They will be dozing off here and there, especially during stage 3.
- Running some performance tests, such as typing accuracy and speed, can to some extent tell your SWS status. In fact, the amount of errors you make (that you usually do not) can ring a bell.
- Checking your learning capabilities with flashcards and different types of knowledge can be helpful. Because explicit/declarative memories directly relate to SWS, examples include past knowledge or academic materials. This long-term memory type demands conscious thought that helps you recollect previous concepts or learned materials.
- Schizophrenia-like symptoms include hallucinations, disordered motor organization and disorganized speech or thinking. Severe and prolonged SWS deprivation can indeed invite these symptoms, so be on the lookout!
- Insulin sensitivity and glucose tolerance may not be immediate to tell. However, you can examine if your diet drastically changes and you cannot control your hunger. Feeling more hungry than usual is a possible sign for lack of SWS.
- Lowered pain threshold and decreased testosterone will affect your training. Thus, you will experience more pain than usual, and cannot exert as much as you normally would.
- SWS reduction slows down muscle recovery rate with lowered growth hormone secretion. Many polyphasic sleepers have in fact experienced this during their adaptations.
- SWS rebounds and instability can affect melatonin secretion pattern. This in return affects REM sleep regulation as well.
- Increased blood pressure can cause nosebleeds, migraines, chest pain, vision issues and irregular heartbeat to name a few. There has been a Dymaxion sleeper with constant nosebleeds while he was adapting!
Selective REM Deprivation
Sleep Architecture
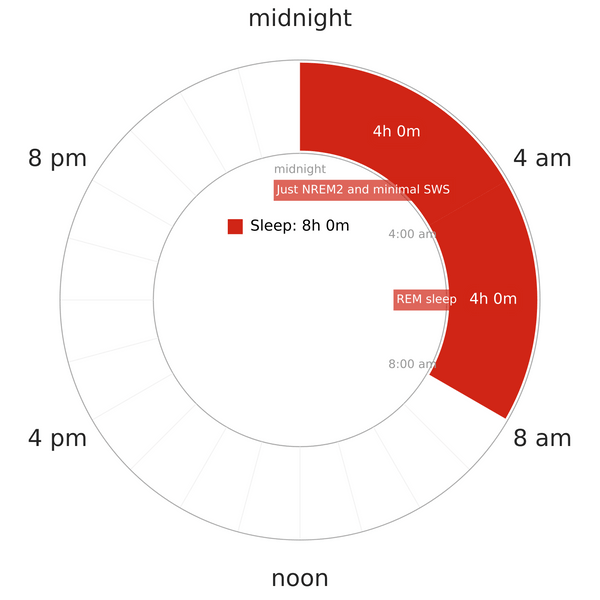
Contrary to selective SWS deprivation, REM deprivation alone seems natural with a shortened monophasic pattern. However, it is usually the case that a core sleep of ~4-5h will still let in some small amount of REM. This type of sleep deprivation is also extremely common in a lot of busy lifestyles today.
Since people usually get some hours of sleep at night, their SWS baseline likely remains intact. Their REM, however, often suffers from the reduction. REM sleep is also known to be more dense around sunrise hours. It is common to experience REM deprivation on any reducing polyphasic schedules with a core sleep long enough to cover all SWS from the beginning.
Effects on Health
Similar to SWS deprivation, some of these study results are not absolute. Some of them will also pave the way for long-term REM deprivation effects. See REM deprivation effects below.
- Hindered consolidation of explicit explicit verbal episodic memories4
- Immunoglobulin A (IgA), an antibody blood protein, decreases in quantity and affects human’s immune profile13.
- Impaired emotional memory consolidation14. Nonetheless, this effect is only apparent in SWS-deprived subjects. In addition, another study showed that this detriment did not affect young, healthy subjects15.
- Diminished selective and automatic attention resources16.
- Enhanced emotional reactivity17.
- Compromised muscle regeneration18. Though this study focuses on rats, there is preliminary evidence pointing toward shift workers and muscle recovery post-injury. This is because shift-workers often have terrible sleep quality.
- Enhanced sensitivity to pain19. However, this conclusion has garnered contradictory results; one such result is SWS deprivation that has more effects.
Cautions for Polyphasic Sleepers
REM sleep is a vital sleep stage for a reason. Thus, before thinking that REM is not as important as SWS, see the cautions below.
- Emotional reactivity refers to the inclination to experience frequent intense emotional arousal. As a result, it may trigger outbursts, bad mood and uncontrollable aggression.
- Also, emotional memory includes any memories or experiences that evoke an emotion. Failure to consolidate this type of memory may cause long-term memory recall issues.
- Verbal episodic memories point to personal experiences or events. From this study, however, short-term REM or SWS deprivation does not weaken implicit verbal memories.
- The potentially degraded immune system especially during adaptations to extreme schedules can initiate sickness. This also means a full recovery on the spot.
- Testosterone contributes to muscle strength, regulates bone mass, fat distribution, red blood cells and sperm to name a few. As a result, lack of REM sleep, where testosterone secretion peaks, will affect muscle gains and personal sex life.
- Although sensitivity to pain may vary among individuals, frequently checking your physical recovery is a good idea.
- Similar to SWS, it is common to microsleep with insufficient REM. There is a hypothesis as follows: SWS improves the unitary motor neuronal components of the attention system, while REM is for the coordination, or connection between such components16.
Implications for Polyphasic Sleep Schedules
Biphasic Sleep
- For reducing variants, REM sleep will be at stake as adaptation starts. If REM requirement can be fulfilled, then the adaptation process is complete just like other schedules.
- Segmented sleep behaves the same as a Dual Core/Multi-core schedule. Waking up right in the middle of the night with the first core sleep can be tricky. However, thanks to its total sleep, its adaptation is a lot easier. See the next section.
- The reason why certain individuals cannot fully adapt to a reducing Biphasic pattern is because of their heightened REM requirement.
Everyman vs Dual/Multi-core
Based on the studies, we can draw some correlations about why certain polyphasic schedules are harder to adapt to than others.
The first common thing is that Dual Core or multi-core schedules are harder than Everyman schedules. We also assume normal sleep requirements (90m REM and 90m SWS daily). Excluding personal sleep preference (natural Segmented sleepers) and complete adaptations, here are some explanations.
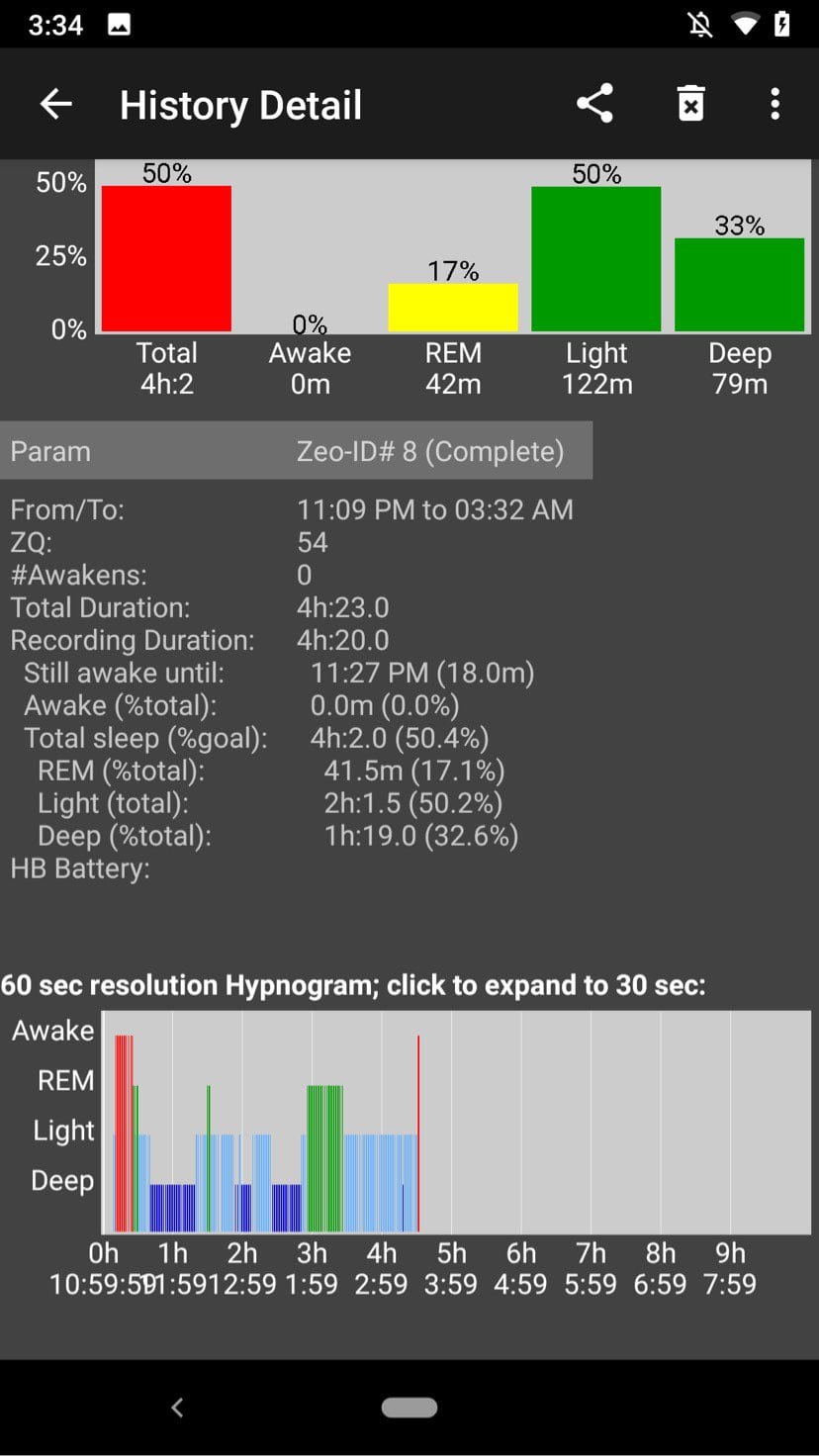
- Dual Core/Multi-core schedules (barring variants with a 4.5h first core) often cannot cover all SWS requirement at the beginning. As a result, SWS deprivation persists until the next core sleep(s), where the circadian rhythm favors REM sleep.
- The wake gap between each core of these schedules are often overwhelming as adaptation progresses.

- Sustaining wakefulness until the next core is difficult with less SWS and REM sleep in the first core.
- For example, the first core of DC3 above (1.5h) does not have much REM sleep, and still fails to cover all SWS baseline. As adaptation progresses, lack of both vital sleep stages will inevitably result in microsleeping and great troubles to stay awake after this core.
- This DC3 sleeper just transitioned to the standard DC3 variant from her adapted E3 (3.5h core). Hence the somewhat repartitioned cores.
- Multi-core schedules need to repartition both SWS and REM into cores and nap(s) accordingly to reach an equilibrium.
- Everyman schedules (barring variants with less than a ~4-4.5h core) have already covered all SWS needs of the day. Apparently, as adaptation goes on with REM rebounds in the core, SWS wakes from the main core still ensue. However, overall, it is easier to meet all SWS requirements with a decently long core sleep from the beginning of adaptation. Therefore, certain Everyman variants only need to repartition REM sleep in the core and the naps.
Other Notes
- Overall, repartitioning of vital sleep on Dual Core/Multi-core schedules is more intense than Everyman sleep. However, note that this difficulty level becomes very different once an Everyman core is less than 2-3 cycles long.
- For example, E3 and E4 will be just as difficult as any regular Dual Core/Multi-core schedules. They will have to repartition both REM and SWS into the core and the naps more intensely. Hence, light sleep percentage will have to further reduce to very low amounts to accommodate this adaptation process.
Nap-only Schedules
- Because of the low amount of sleep, it is normal to run into intense SWS and REM deprivation symptoms. Each nap can only provide some small portion of REM, SWS, or both.
- Thanks to SWS’ quick rebounds, it is very easy to oversleep any naps. Additionally, staying awake until the next nap is going to be hellish due to intensified SWS and REM deprivation.
- Nap-only schedules overall give no solid clues about which nap(s) will contain primarily SWS or REM sleep. The avalanche of homeostatic pressures of both REM and SWS makes things highly unpredictable.
- The general failure of these schedules to support average humans’ sleep need means that the adaptation period likely will stagnate.
Main author: GeneralNguyen
Page last updated: 10 April 2021
Reference
- Lentz, Martha J., et al. “Effects of selective slow wave sleep disruption on musculoskeletal pain and fatigue in middle aged women.” The Journal of rheumatology 26.7 (1999): 1586-1592. [PubMed]
- Hsu, C., et al. “0251 THE EFFECT OF SLOW WAVE SLEEP DEPRIVATION ON ERROR MONITORING.” Sleep 40 (2017): A92. [PubMed]
- Li, Yun, et al. “Deficits in attention performance are associated with insufficiency of slow-wave sleep in insomnia.” Sleep medicine 24 (2016): 124-130. [PubMed]
- Casey, Sarah J., et al. “Slow wave and REM sleep deprivation effects on explicit and implicit memory during sleep.” Neuropsychology 30.8 (2016): 931. [PubMed]
- Kundermann, Bernd, et al. “The effects of sleep deprivation on pain.” Pain Research and Management 9.1 (2004): 25-32. [PubMed]
- Ukraintseva, Yu V., et al. “Slow-wave sleep and androgens: selective slow-wave sleep suppression affects testosterone and 17α-hydroxyprogesterone secretion.” Sleep medicine 48 (2018): 117-126. [PubMed]
- Ferrara, Michele, et al. “Selective slow‐wave sleep deprivation and time‐of‐night effects on cognitive performance upon awakening.” Psychophysiology 37.4 (2000): 440-446. [PubMed]
- Van Der Werf, Ysbrand D., et al. “Reduction of nocturnal slow-wave activity affects daytime vigilance lapses and memory encoding but not reaction time or implicit learning.” Progress in brain research 193 (2011): 245-255. [PubMed]
- Sarkar, Sukanto, et al. “Slow wave sleep deficits as a trait marker in patients with schizophrenia.” Schizophrenia research 124.1-3 (2010): 127-133. [PubMed]
- Ukraintseva, Yu V., et al. “Selective slow-wave sleep suppression affects glucose tolerance and melatonin secretion. The role of sleep architecture.” Sleep medicine 67 (2020): 171-183. [PubMed]
- Shaw, Natalie D., et al. “Effect of slow wave sleep disruption on metabolic parameters in adolescents.” Sleep 39.8 (2016): 1591-1599. [PubMed]
- Sayk, Friedhelm, et al. “Effects of selective slow-wave sleep deprivation on nocturnal blood pressure dipping and daytime blood pressure regulation.” American Journal of Physiology-Regulatory, Integrative and Comparative Physiology 298.1 (2010): R191-R197. [PubMed]
- Ruiz, Francieli S., et al. “Immune alterations after selective rapid eye movement or total sleep deprivation in healthy male volunteers.” Innate immunity 18.1 (2012): 44-54. [PubMed]
- Wiesner, Christian D., et al. “The effect of selective REM-sleep deprivation on the consolidation and affective evaluation of emotional memories.” Neurobiology of learning and memory 122 (2015): 131-141. [PubMed]
- Morgenthaler, Jarste, et al. “Selective REM-sleep deprivation does not diminish emotional memory consolidation in young healthy subjects.” PloS one 9.2 (2014): e89849. [PubMed]
- Zerouali, Younes, Boutheina Jemel, and Roger Godbout. “The effects of early and late night partial sleep deprivation on automatic and selective attention: An ERP study.” Brain research 1308 (2010): 87-99. [PubMed]
- Rosales-Lagarde, Alejandra, et al. “Enhanced emotional reactivity after selective REM sleep deprivation in humans: an fMRI study.” Frontiers in behavioral neuroscience 6 (2012): 25. [PubMed]
- Mônico-Neto, Marcos, et al. “REM sleep deprivation impairs muscle regeneration in rats.” Growth Factors 35.1 (2017): 12-18. [PubMed]
- Azevedo, Eduardo, et al. “The effects of total and REM sleep deprivation on laser-evoked potential threshold and pain perception.” Pain 152.9 (2011): 2052-2058. [PubMed]
