Introduction
A sleeper with non-24h circadian rhythms is someone with a “free-running” sleep schedule. In fact, scientists consider free-running sleep a type of circadian rhythm disorder, free-running disorder (FRD). Typically though, these individuals have a longer circadian rhythm than the regular 24h we know about.
If you have heard about delayed sleep phase disorder, you probably know about non-24h cases. For example, there have been documented cases on 25h, 26h or up to ~28h circadian rhythm. Over the years, we have also seen few individuals with FRD join the community in hope of improving their sleep quality. This post will examine the behavior of a non-24h circadian rhythm in humans and its viability in polyphasic sleeping.
NOTE: Because of the scarcity of information on non-24h rhythm, we only present some of the most relevant pieces of literature. Furthermore, we will only discuss sighted individuals. Blind people, on the other hand, have a natural tendency for a non-24h sleep pattern.
Definition & Characteristics of a Non-24h Circadian Rhythm
For the scope of this post, we will only focus on free-running sleep, the most common prototype of non-24h rhythm.
To start, a trademark non-24h circadian rhythm involves an intrinsic circadian period that is consistently longer than 24 hours1.
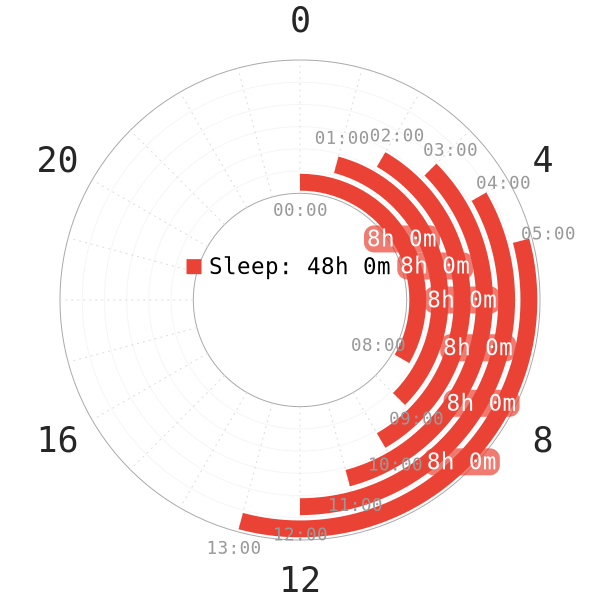
- In specifics, sleepers suffering from this sleep disorder delay their sleep on a nightly basis.
- The start of sleep times becomes later and later as days go on. Likewise, wakeup time also moves back each day.
- After approximately a couple weeks, the bedtime cycles back to the original start time.
- Free-running sleep bears striking resemblances to sleep patterns in time-free environments1. What this means is that when there are no time cues for sleep, human sleep follows the non-24h circadian rhythm naturally.
- While humans generally have a slightly longer than 24h circadian rhythm, the standard deviation value is not significant. Usually, it hovers around 24.15h on average1.
Effects of Non-24h Rhythm on Health
Detriments
Going by the currently available data, very few healthy individuals can sustain free-running sleep2. Furthermore, non-24h sleep can seriously do damage on health and well-being.
- In a large sample of 57 patients with FRD, a high portion (25%) of patients also have psychiatric disorders1.
- Two out of four sleepers in Antarctica from a 1-year sleep study3 secreted more cortisol than normal.
- Even though they maintained good enough overall health, their mood and interpersonal relationships suffered. However, it is worth noting that the free-running rhythm was only present with the sun below the horizon.
- For the other time periods of the year, these sleepers automatically re-entrained with the normal 24h circadian rhythm.
- Puredoxyk, a veteran polyphasic sleeper, also explained the utter inconvenience of free-running sleep4. Specifically, free-running sleep is extremely impractical for regular 9-to-5 or conventional occupations. Microsleeps, fatigue, psychological complaints, chronic sleep deprivation are all prevalent5.
- Despite indirect evidence, disruptions in the circadian rhythm can develop cancer6. This is because the circadian rhythm shows a consistent 24-hour rhythmic period in almost all species6. Therefore, free-running sleep, a desynchronized rhythm, at least has some potential risks for cancer development.
- Consistently advanced or delayed phase in free-running rhythm indirectly can result in type-2 diabetes and obesity7. Circadian misalignment, therefore, can contribute to low insulin sensitivity. The results are from experimenting on a 21h and 27h circadian rhythm short-term.
Based on all these elements, while free-running sleep may be natural in non-24h individuals, the possible long-term effects should not be overlooked.
How to Adapt to a 24h Circadian Rhythm
Treatments for non-24h rhythm have been available and worked to some extent. This is also something you should pay attention to, before starting a polyphasic schedule. A couple self-reported non-24h polyphasic sleepers have been able to adapt to a normal 24h polyphasic schedule by utilizing the light-dark cycle.
Below are some of the methods that can help create a 24h circadian rhythm8:
- Light therapy
- Chronotherapy
- Vitamin B12
- Timed melatonin administration1
- Prescribed sleep-wake scheduling by introducing more time cues1
NOTE: These methods may still not work for all non-24h sleepers.
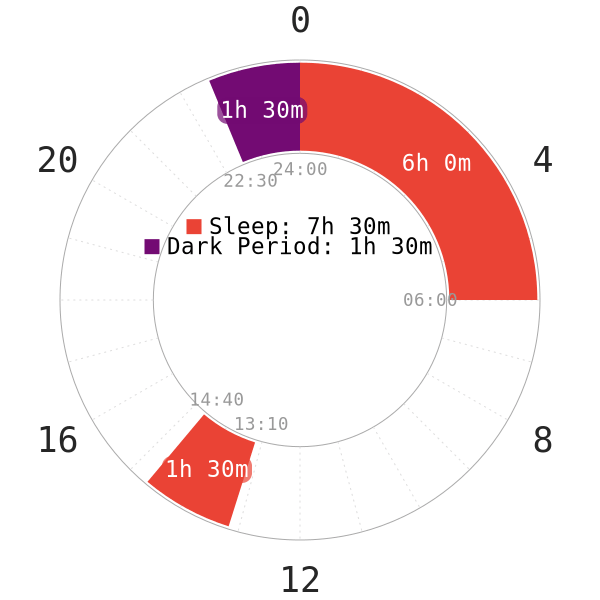
Specifically, the last method has worked for adapted polyphasic sleepers who were originally non-24h sleeper. This is also similar to our very recommended Dark Period course. We have detailed different means to keep a polyphasic schedule conformed to the 24h circadian rhythm. Such time cues, such as breakfast timing, no blue lights before nocturnal sleep and exercising all play into the equation.
By reverting to the normal circadian timing, these sleepers have been able to adapt to some moderate polyphasic schedules. For example, Segmented, Siesta and DC1. On the other hand, there has been zero successful adaptation to any non-24h polyphasic patterns. There have certainly been attempts, but all led to failure, even with non-reducing schedules.
Sleep Architecture of Non-24h Circadian Rhythm
- The nocturnal rhythm of melatonin production is present even with non-24h sleep schedules9.
- This observation therefore suggests that it is possible to dedicate a longer sleep episode around melatonin secretion peak.
- Melatonin surge also defines the duration of the biological night9.
- REM sleep regulation is very different on a free-running rhythm than a regular 24h rhythm10.
- Specifically, REM sleep appears in all sleep cycles of a non-24h core sleep rather than concentrated around only sunrise hours in 24h rhythm.
- Free-running rhythm also forms many temperature minima during sleep, with the preference for the first and last sleep cycle. Therefore, it may explain why polyphasic sleepers wake up feeling cold from a REM-filled sleep block in the early morning hours.
- Because of REM sleep’s strong propensity in the early sleep cycles, it may contribute to a lower amount of SWS in at least the first sleep cycle.
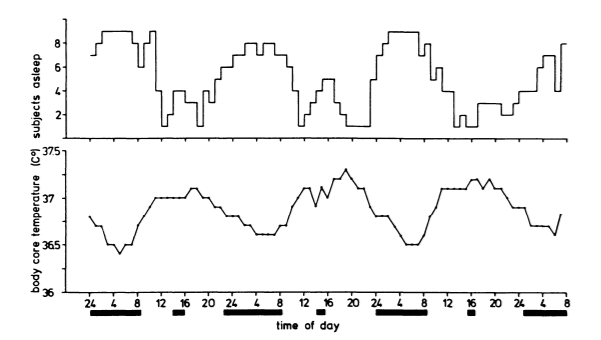
- Daytime naps and core sleeps have a clear relationship with core body temperature11. Based on a very short-term study:
- Even in non-24h rhythm, 23/26 naps often occur when body temperature is at or near maximum. This surprisingly coincides with the regular afternoon (siesta-type) naps, where our body temperature reaches the highest.
- Likewise, nocturnal sleep bouts are natural with minimum body temperature.
- Napping is one supplemental component of the circadian system; thus, it also reflects the timing of the circadian pacemaker of sleep and wakefulness.
Implications for Polyphasic Sleep
There are indirect correlations for polyphasic sleep with all the presented information. However, note that these are mostly speculations or recommendations.
- Some sort of non-reducing Biphasic sleep with the timing of body temperature may be adaptable or even natural for non-24h sleepers. This recommendation also assumes they work at home and can sleep whenever they want. Typically, something with a long sleep session and an extra nap in theory can work out.
- It is generally a bad idea to place short naps at nocturnal hours. This is because of potential SWS wakes and the preference for core sleep placements.
- Time-free sleep environments are sometimes mandatory, regardless of our desires. For example, space missions typically desynchronize circadian time cues. Under these conditions, adding naps can still help with performance and body functions12.
- Due to the complicated regulations of body temperature and REM sleep, a multi-core schedule may not be suitable or effective for non-24h sleepers.
- The effective success rate of non-24h polyphasic schedules up to date remains nonexistent. Unfortunately, it is unknown how the traditional concepts would apply under time-free conditions.
- Reducing polyphasic schedules can even further modify sleep stage regulations under a time-free environment. Eventually, they can totally overwhelm any attempts to conform to a specific sleep duration.
Conclusion
Non-24h circadian rhythm poses huge future risks and is a debilitating sleep disorder. However, there is still some hospitability with the napping culture. There are also possible treatments that have thoroughly changed sleep quality of certain non-24h sleepers. As a result, returning to the normal circadian rhythm and adapting to a conventional polyphasic sleep pattern are viable. The concept of core body temperature may just be the first guideline for reducing tiredness and improving sleep efficiency.
While there are certainly negative health effects of a non-24h circadian rhythm, more long-term evidence is necessary.
Main author: GeneralNguyen
Page last updated: 5 March 2021
Reference
- Sack, R. L., Auckley, D., Auger, R. R., Carskadon, M. A., Wright, K. P., Vitiello, M. V., & Zhdanova, I. V. (2007). Circadian Rhythm Sleep Disorders: Part II, Advanced Sleep Phase Disorder, Delayed Sleep Phase Disorder, Free-Running Disorder, and Irregular Sleep-Wake Rhythm. Sleep, 30(11), 1484–1501. doi:10.1093/sleep/30.11.1484. [PubMed]
- Kitamura, S., Hida, A., Enomoto, M., Watanabe, M., Katayose, Y., Nozaki, K., … Mishima, K. (2013). Intrinsic Circadian Period of Sighted Patients with Circadian Rhythm Sleep Disorder, Free-Running Type. Biological Psychiatry, 73(1), 63–69. doi:10.1016/j.biopsych.2012.06.027.
- Kennaway, D. J., & Van Dorp, C. F. (1991). Free-running rhythms of melatonin, cortisol, electrolytes, and sleep in humans in Antarctica. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology, 260(6), R1137–R1144. doi:10.1152/ajpregu.1991.260.6.r1137. [PubMed]
- Puredoxyk. Ubersleep : Nap-Based Sleep Schedules and the Polyphasic Lifestyle. United States, Puredoxyk, 2013.
- American Academy of Sleep Medicine (2001). The International Classification of Sleep Disorders, Revised (ICSD-R)(PDF). ISBN 978-0-9657220-1-8.
- Savvidis, C., & Koutsilieris, M. (2012). Molecular Medicine, 18(9), 1. doi:10.2119/molmed.2012.00077.
- Gonnissen, H. K. J., Mazuy, C., Rutters, F., Martens, E. A. P., Adam, T. C., & Westerterp-Plantenga, M. S. (2013). Sleep Architecture When Sleeping at an Unusual Circadian Time and Associations with Insulin Sensitivity. PLoS ONE, 8(8), e72877. doi:10.1371/journal.pone.0072877. [PubMed]
- Dagan, Y., & Abadi, J. (2001). SLEEP-WAKE SCHEDULE DISORDER DISABILITY: A LIFELONG UNTREATABLE PATHOLOGY OF THE CIRCADIAN TIME STRUCTURE. Chronobiology International, 18(6), 1019–1027. doi:10.1081/cbi-100107975. [PubMed]
- Blask, D. E. (2009). Melatonin, sleep disturbance and cancer risk. Sleep Medicine Reviews, 13(4), 257–264. doi:10.1016/j.smrv.2008.07.007. [PubMed]
- Jürgen, Z. (1980). Distribution of REM Sleep in Entrained 24 Hour and Free-Running Sleep-Wake Cycles. Sleep, 2(4), 377–389. doi:10.1093/sleep/2.4.377. [PubMed]
- Stampi, Claudio. Why We Nap : Evolution, Chronobiology, and Functions of Polyphasic and Ultrashort Sleep. Birkhauser, 2014.
- Mallis, M. M., and C. W. DeRoshia. “Circadian Rhythms, Sleep, and Performance in Space.” Aviation, Space, and Environmental Medicine 76.6 (2005). [PubMed]
