Introduction
Although seemingly irrelevant, there is actually some relationship between schizophrenia and sleep. However, a lot of findings may appear controversial regarding this specific psychiatric disorder. Moreover, like many other topics, there are no direct research or experiments between polyphasic sleeping and schizophrenia.
Because of the indirect research outcomes, this post will only serve to certain precautions for desired polyphasic sleepers. We hope that there will be more extensive research on the potential or any other negative aspects of polyphasic sleeping.
Classification of Schizophrenia
Symptoms
Schizophrenia actually has a long history as a medical condition. Although there are different types, such as: catatonic, paranoid, etc. there are 2 main symptoms1:
- Positive symptoms: Usually changes in behavior or thoughts, such as hallucination and delusion
- Negative symptoms: “Flattened” emotion, which is about withdrawal from the world, no interest in daily social interactions.
Assessments may vary, and depending on the severity, each symptom may be overwhelming or not. However, negative symptoms often appear more complicated to treat than positive equivalents. While positive symptoms do not predict any specific outcomes other than further hospitalization, negative symptoms can critically affect multiple aspects of quality of life1. This includes global daily functions, bad mood like anxiety, work and social performance.
Aside from these conditions, schizophrenic patients also often have high rates of comorbidity. Examples include: diabetes and cardiovascular diseases2.
Sleep Structure and Quality
Both symptoms, overall show negative sleep quality in patients3. Below are the relevant observations in a meta-analysis3:
- Negative symptoms are heavily associated with abnormally low SWS duration, especially from patients who first withdraw from antipsychotic medications. Furthermore, this also indicates thalamocortical dysfunction.
- Increased sleep onset duration
- Reduced sleep spindles activity, which results in sleep-dependent motor learning failure.
- Decreased total sleep time
- Plummeted sleep efficiency
- Increased total awake time. This means that schizophrenic patients often have very long WASO duration.
Polyphasic Sleep’s Roles in Well-Being
Sleep Stages and Their Importance
- A reduction in quantity of sleep spindles, which are present in both NREM2 and SWS, has been linked to schizophrenia and the development of schizophrenia-like symptoms4,5,6,7,8.
- However, it is noteworthy that longer sleep duration and higher sleep efficiency have a negative correlation with neutrophil counts, which are markers for inflammation2.
- Schizophrenic patients sleep 32% longer than the healthy group. However, their sleep quality is very poor and they have troubles getting deeper sleep.
- Sleep efficiency is defined as the ratio of NREM2, SWS and REM duration per total sleep time. Thus, higher sleep efficiency can simply mean more NREM2 duration (actual sleep but not truly restful sleep). As a result, this parameter alone can be misleading.
Implications for Polyphasic Sleeping
Because of the unorthodox nature of polyphasic sleep, you may pose questions of whether it can develop schizophrenia. First and foremost, healthy polyphasic sleep accommodates for the full SWS and REM needs of people after adapting. For the most part, the total sleep is usually at least 4-5 hours. Thus, this should not cause concerns for schizophrenic symptoms.
However, the same may not apply to nap-only schedules. This is because the radically restrictive total sleep can directly affect the amount of available sleep spindles that are necessary for well-being. However, currently, there is no concrete research on the minimum amount of recommended daily sleep spindles and NREM2 duration.
The reason why this should not concern healthy polyphasic schedules is because they do not reduce the amount of SWS people gain each day. Specifically, the sleep spindles from SWS and the small reduction in NREM2 after adapting seem enough to not trigger schizophrenic developments.
Polyphasic Sleep Anecdotes
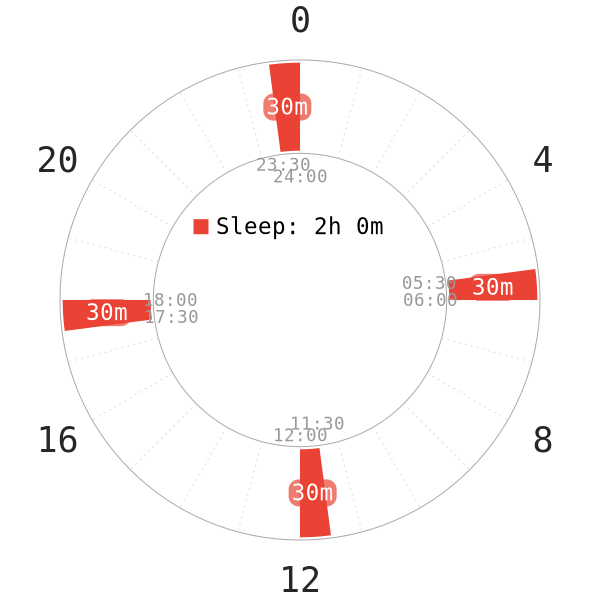
- On nap-only schedules, average humans do not get enough SWS. As a result, this is bound to increase the risk of these symptoms. Here is a Reddit post of a person who was on the Tesla sleep schedule for 8 months.
- Another polyphasic sleeper in the Discord who suffers from schizophrenic personality disorder was able to adapt to Dymaxion short-term.
- She is also a moderate insomniac in her words, and have trouble falling asleep on any sleep patterns.
- Additionally, she was potentially a short sleeper, or chronically sleep deprived because of the naturally short sleep duration.
- Finally, she stayed on the schedule for 3 more months before falling sick. However, it was because of a flu rather than the schedule itself. Regardless, it is also unknown if Dymaxion indirectly increased her vulnerability to flu and sickness in general.
- She still had sleep onset issues with her own sleep after switching to a less extreme schedule afterwards, however.
- Overall, her daily performance on Dymaxion was reportedly the same as on her normal sleep schedule.
Treatments of Schizophrenia
However, schizophrenia remains incurable as of the current date. While it is possible to mitigate certain symptoms, sufferers still have to live with this disorder for their lifetime. Regarding possible future treatments of schizophrenia, interestingly enough, temporary sleep restriction was proposed as a possible solution9. According to this proposal:
- There are similarities between sleep deprivation and schizophrenia. For example, hallucinations and certain negative symptoms in schizophrenia.
- Sleep restriction model in combination with other schizophrenic models may be a sensible strategy. Such models include the use of ketamine.
- It is also possible that sleep restriction strategies can force deeper overall sleep and reduce sleep onset.
Other than these points, no research thus far has carried out this proposal. Even though sleep restriction is similar to polyphasic sleeping, this is NOT our medical advice. Consult your physician about your conditions.
Regardless, very few people have noticed mild symptoms of schizophrenia, like paranoia and the feeling of not being alone when adapting to healthy polyphasic schedules. After the adaptation is complete, these symptoms quickly subside, leaving no damage at all.
Main authors: Crimson & GeneralNguyen
Page last updated: 15 February 2021
Reference
- Fenton, W. S. (1991). Natural History of Schizophrenia Subtypes. Archives of General Psychiatry, 48(11), 978. doi:10.1001/archpsyc.1991.01810350018003.
- Fang, S.-H., Suzuki, K., Lim, C. L., Chung, M.-S., Ku, P.-W., & Chen, L.-J. (2016). Associations between sleep quality and inflammatory markers in patients with schizophrenia. Psychiatry Research, 246, 154–160. doi:10.1016/j.psychres.2016.09.032.
- Chan, M.-S., Chung, K.-F., Yung, K.-P., & Yeung, W.-F. (2017). Sleep in schizophrenia: A systematic review and meta-analysis of polysomnographic findings in case-control studies. Sleep Medicine Reviews, 32, 69–84. doi:10.1016/j.smrv.2016.03.001. [PubMed]
-
Ferrarelli F, Peterson M, Sarasso S, et al. Thalamic dysfunction in schizophrenia suggested by whole-night deficits in slow and fast spindles. Am J Psychiatry. 2010;167(11):1339-1348. [PubMed]
- Seeck-Hirschner M, Baier P, Sever S, Buschbacher A, Aldenhoff J, Göder R. Effects of daytime naps on procedural and declarative memory in patients with schizophrenia. J Psychiatr Res. 2010;44(1):42-47. [PubMed]
-
Manoach D, Thakkar K, Stroynowski E, et al. Reduced overnight consolidation of procedural learning in chronic medicated schizophrenia is related to specific sleep stages. J Psychiatr Res. 2010;44(2):112-120. [PubMed]
- Tesler N, Gerstenberg M, Franscini M, Jenni O, Walitza S, Huber R. Reduced sleep spindle density in early onset schizophrenia: a preliminary finding. Schizophr Res. 2015;166(1-3):355-357. [PubMed]
- Göder R, Graf A, Ballhausen F, et al. Impairment of sleep-related memory consolidation in schizophrenia: relevance of sleep spindles? Sleep Med. 2015;16(5):564-569. [PubMed]
- Kumari, V., & Ettinger, U. (2020). Controlled sleep deprivation as an experimental medicine model of schizophrenia: An update. Schizophrenia Research. doi:10.1016/j.schres.2020.03.064. [PubMed]
