Introduction
Slow-wave Sleep (SWS), often also referred to as NREM3 or Deep Sleep, is a crucial sleep stage in humans. In the past, there were 2 separate stages of deep sleep, namely Stage 3 and Stage 4. However, as of 2007, SWS only consists of one stage, which is stage 31. This is because there is only some minor difference between the previous stages 3 and 42. Likewise, stage 1 and 2 are light sleep.
In the history of polyphasic sleeping, the functions of SWS have unfortunately been largely overlooked. Because REM sleep was the primary focus, it has left a big information gap on how SWS affects the body that many people may not know. In this post, you will learn about the functions of SWS and its importance for polyphasic sleepers.
Characteristics of Deep Sleep
There are many unique features of deep sleep that sets it apart from other sleep stages. In addition, these details will serve to relay information and understanding of SWS in the context of polyphasic sleeping. This section will examine the various aspects of this sleep stage.
NREM Sleep Behavior
Being part of the NREM sleep category, SWS inherits most of the core traits, with some notable differences.
- The most noticeable feature of SWS is the increased slow-wave activity, which facilitates most of the bodies restorative functions when it is resting.
- In addition, SWS is the hardest sleep stage to wake from. This thus increases the chance to completely miss an alarm altogether during this stage.
- Both the cerebral blood flow and cerebral metabolic rate are reduced much more during SWS than during NREM23.
- Because SWS is the deepest sleep stage, dream recall is often very murky. However, it is still possible to recall dreams from SWS. Usually though, the dream contents are often ambiguous and much less vivid than those during REM sleep5.
- The most active regions of an awake brain have the highest level of delta waves during SWS. Since the brain “shuts down”, people woken during this stage often experience grogginess, brain fog, and headaches. This is because it takes time for the cerebral cortex to resume its normal functions. See sleep inertia.
Vital Bodily Functions of Deep Sleep
Without a doubt, SWS is basically the most important sleep stage in humans. Though humans are asleep, multiple important bodily processes are still occurring, especially during this sleep stage. Consequently, it is important to understand these activities and the consequences of not getting enough deep sleep in the long-term.
Restorative Functions
- Endocrine and cardiovascular activities: Growth hormone secretion often peaks during this sleep stage6. This is especially critical for teenagers who are still growing and physically active individuals.
- Parasympathetic nervous system: Deep sleep ensures the shift of the autonomic nervous system to the parasympathetic nervous system7. Therefore, it is important to wind down before sleep to assist the body with deactivating the flight-or-fight responses. Additionally, this process would improve overall sleep quality.
- Declarative memories: This is another hallmark role of deep sleep. We also know that sleep is necessary for memory formation, and deep sleep consolidates declarative memories8. Additionally, this type of memory is also called explicit memory. Specifically, it is the recollection of factual information, previous experiences and concepts.
- Immune functions and glial cell recovery9: Apparently, lack of SWS will only reduce immune functions and disrupts glial cell restoration.
- Repairing and healing muscles: There is potentially an increase in deep sleep amount after a heavy exercise or workout10. However, it may still depend on individuals and the intensity of exercising.
- Brain waste removal: In fact, one of the most important functions of SWS is the removal of metabolic waste products from the brain by the glymphatic system11. During this sleep stage, the brain cells shrink in size to foster the removal of the potentially neurotoxic intracranial fluid.
Consequences of Inadequate Deep Sleep
Over time, there has been a lot of documentation of insufficient deep sleep long term. Most notably, the consequences include, but not limited to:
- Hypertension12
- Alzheimer’s disease13
- Type 2 diabetes14
- Stunted growth15
- Weakened immune system9
It is also worth noting that a lot of individuals with depression, schizophrenia and bipolar also usually have an abnormally low amount of daily SWS requirements16,17. However, the findings remain somewhat controversial with schizophrenia.
How Much Deep Sleep to Get Daily?
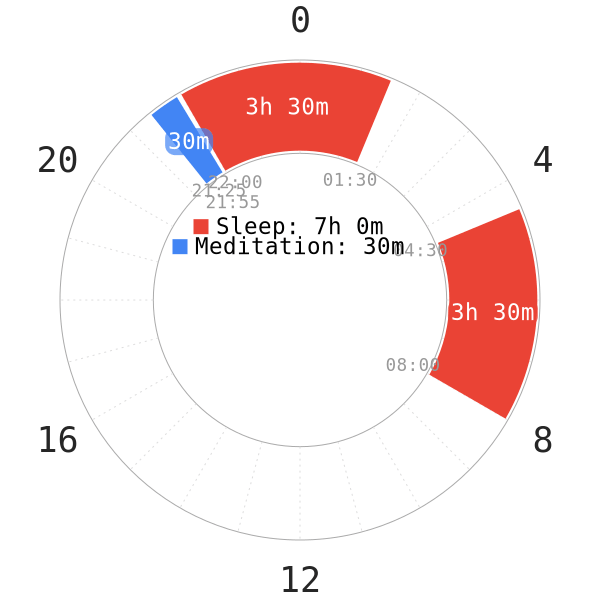
Ever since the industrial era began, humans have shifted from the common Segmented sleep pattern to monophasic sleep. Ever since, monophasic sleep has become the most popular sleep pattern today. However, SWS only accounts for a fraction of the amount of total sleep.
- Under regular, nocturnal monophasic conditions, specialists often recommend an average of 90m SWS each day, or 80-120m depending on individuals. This translates to approximately ~20-25% of a normal 7-8h monophasic sleep2.
- There are also normal adults who perpetually receive lower daily SWS, only around ~10% of total sleep time2; however, this is mostly typical in the elderly.
- A lot of teenagers, physically active individuals or high-SWS-requirement individuals may require at least 120m of daily SWS for optimal performance.
- It is also intriguing to note that short sleepers, those who often have shorter monophasic duration than average without any psychological issues, have basically the same amount of SWS as normal and long sleepers18. However, their REM and light sleep duration is less than those of normal sleepers.
NOTE: Your personal SWS baseline may be a bit more or less than the average values (e.g, 70m of daily SWS). If you have dedicated sleep tracking devices and those are your natural SWS baseline values, you may fare well even with a somewhat lower than the recommended values.
Nowadays, the prevalence of blue lights before nocturnal sleep has caused a decline in SWS amounts of a lot of people; this in return results in lack of vigor and unrestful awakening in the morning. Hence, it is only necessary to delve into the possible factors that contribute to SWS reduction in humans.
Factors that reduce deep sleep
Since certain factors are largely unknown or unclear, we will only detail very common contributors.
- Blue light exposure before bedtime. As a result, this delays melatonin onset and impacts the vital sleep stages negatively. See the Dark Period Course for more information.
- Even dim artificial light exposure during sleep time also disrupts deep sleep and even inflates light and REM sleep duration19. Therefore, it is very important, if not the most ideal, to sleep in complete darkness.
- A poor diet, namely high sugar intake, low fiber and high saturated fat20. This is obvious, as garbage food degrades SWS quality.
- Stress and anxiety. Both make it difficult to sleep deeply. In fact, they cause more abrupt wakes at night and disrupt SWS21. Hence, it is even more crucial for polyphasic sleepers to manage stress levels.
- Obstructive sleep apnea22
- Age. The elderly have much less SWS in their sleep than younger adults.
- Narcolepsy.
Factors that increase deep sleep
If total daily SWS is unusually lower than the baseline value and causes poor sleep quality, there are certain options to improve SWS duration safely.
- Magnesium23
- Increase exercise intensity and frequency
- Valerian24
- Gabapentin25
- Alcohol26
- Very low-carb diets27
- A well-rounded diet
- A well-maintained dark period
- Sickness or injury
- Age. Mentally and physically growing teenagers can have bursts of increased SWS.
Identifying SWS from an EEG reading
If you don’t own an EEG, you do not need to pay attention to this section. This is because it only helps people understand how to identify whether a sleep block they had and recorded contained any SWS.
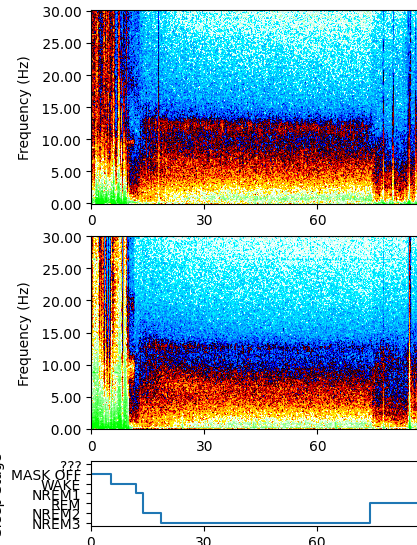
- Using standard criteria, the amplitude, frequency and bursts of low-frequency oscillations are less than 2 Hz in an EEG device2.
- Even though sleep spindles are present during all NREM sleep stages, deep sleep do not contain as much sleep spindles as NREM2. Rather, it mostly consists of slow-waves4.
Conclusion
There are many yet-to-be discovered mechanics regarding deep sleep. However, its current behavior in a 24-hour circadian rhythm has hidden potentials for polyphasic sleepers to tap into. Regardless of sleep patterns, though, being unable to sustain a personal SWS requirement daily will result in a cumulative downfall in health and well-being. Deep sleep is, and always will play an important role in optimizing performance of the brain and the body.
Main author: GeneralNguyen
Olimex image by: Dakyne
Page last updated: 19 January 2021
Reference
- NOVELLI, L., FERRI, R., & BRUNI, O. (2010). Sleep classification according to AASM and Rechtschaffen and Kales: effects on sleep scoring parameters of children and adolescents. Journal of Sleep Research, 19(1p2), 238–247. doi:10.1111/j.1365-2869.2009.00785.x. [PubMed]
- Dijk, Derk-Jan. “Regulation and functional correlates of slow wave sleep.” Journal of Clinical Sleep Medicine 5.2 suppl (2009): S6-S15. [PubMed]
- Madsen P, Vorstrup S. Cerebral blood flow and metabolism during sleep. Cerebrovasc Brain Metab Rev. 1991;3(4):281-296. [PubMed]
- Dijk DJ, Hayes B, Czeisler CA. Dynamics of electroencephalographic sleep spindles and slow wave activity in men: effect of sleep deprivation. Brain Res 1993;626:190-9. [PubMed]
- Cavallero C, Cicogna P, Natale V, Occhionero M, Zito A. Slow Wave Sleep Dreaming. Sleep. 1992;15(6):562-566. doi:10.1093/sleep/15.6.562. [PubMed]
- Van Cauter E, Latta F, Nedeltcheva A, et al. Reciprocal interactions between the GH axis and sleep. Growth Horm IGF Res2004;14 Suppl A:S10-S17. [PubMed]
- Viola AU, James LM, Archer SN, Dijk DJ. PER3 polymorphism and cardiac autonomic control: effects of sleep debt and circadian phase. Am J Physiol Heart Circ Physiol 2008;295:H2156-H2163. [PubMed]
- Gais, S., & Born, J. (2004). Low acetylcholine during slow-wave sleep is critical for declarative memory consolidation. Proceedings of the National Academy of Sciences, 101(7), 2140–2144. doi:10.1073/pnas.0305404101. [PubMed]
- The importance of sleep & why we need it. Human Givens Institute. https://www.hgi.org.uk/resources/delve-our-extensive-library/dreaming/importance-sleep-why-we-need-it#.U2kpm8fhjys. Published October 23, 2015. Accessed November 4, 2018.
- Vyazovskiy, Vladyslav V. “Sleep, recovery, and metaregulation: explaining the benefits of sleep.” Nature and science of sleep 7 (2015): 171. [PubMed]
- Xie L, Kang H, Xu Q, et al. Sleep Drives Metabolite Clearance from the Adult Brain. Science. 2013;342(6156):10.1126/science.1241224. [PubMed]
- Fung, M. M., Peters, K., Redline, S., Ziegler, M. G., Ancoli-Israel, S., … Barrett-Connor, E. (2011). Decreased Slow Wave Sleep Increases Risk of Developing Hypertension in Elderly Men. Hypertension, 58(4), 596–603. doi:10.1161/hypertensionaha.111.174409. [PubMed]
- Ju, Yo-El S., et al. “Slow wave sleep disruption increases cerebrospinal fluid amyloid-β levels.” Brain 140.8 (2017): 2104-2111.
- Tasali, E., Leproult, R., Ehrmann, D. A., & Van Cauter, E. (2008). Slow-wave sleep and the risk of type 2 diabetes in humans. Proceedings of the National Academy of Sciences, 105(3), 1044–1049. doi:10.1073/pnas.0706446105. [PubMed]
- Sassin, J. F., et al. “Effects of slow wave sleep deprivation on human growth hormone release in sleep: preliminary study.” Life Sciences 8.23 (1969): 1299-1307. [PubMed]
- Hoffmann, R., Hendrickse, W., Rush, A. J., & Armitage, R. (2000). Slow-wave activity during non-REM sleep in men with schizophrenia and major depressive disorders. Psychiatry Research, 95(3), 215–225. doi:10.1016/s0165-1781(00)00181-5. [PubMed]
- Armitage, R., Hoffmann, R., Trivedi, M., & Rush, A. J. (2000). Slow-wave activity in NREM sleep: sex and age effects in depressed outpatients and healthy controls. Psychiatry Research, 95(3), 201–213. doi:10.1016/s0165-1781(00)00178-5. [PubMed]
- Hao, Y. L., et al. “A three-phase epidemiological study of short and long sleepers in a middle-aged Chinese population: prevalence and characteristics.” Brazilian Journal of Medical and Biological Research 47.2 (2014): 157-165. [PubMed]
- Cho, C.-H., Lee, H.-J., Yoon, H.-K., Kang, S.-G., Bok, K.-N., Jung, K.-Y., … Lee, E.-I. (2015). Exposure to dim artificial light at night increases REM sleep and awakenings in humans. Chronobiology International, 33(1), 117–123. doi:10.3109/07420528.2015.1108980. [PubMed]
- St-Onge, M.-P., Roberts, A., Shechter, A., & Choudhury, A. R. (2016). Fiber and Saturated Fat Are Associated with Sleep Arousals and Slow Wave Sleep. Journal of Clinical Sleep Medicine, 12(01), 19–24. doi:10.5664/jcsm.5384. [PubMed]
- Kecklund, G., & Åkerstedt, T. (2004). Apprehension of the subsequent working day is associated with a low amount of slow wave sleep. Biological Psychology, 66(2), 169–176. doi:10.1016/j.biopsycho.2003.10.004. [PubMed]
- Ratnavadivel, Rajeev, et al. “Marked reduction in obstructive sleep apnea severity in slow wave sleep.” Journal of clinical sleep medicine 5.6 (2009): 519-524. [PubMed]
- Durlach, J., et al. “Magnesium and thermoregulation. I. Newborn and infant. Is sudden infant death syndrome a magnesium-dependent disease of the transition from chemical to physical thermoregulation?.” Magnesium Research 4.3-4 (1991): 137-152. [PubMed]
- Donath, F., et al. “Critical evaluation of the effect of valerian extract on sleep structure and sleep quality.” Pharmacopsychiatry 33.02 (2000): 47-53. [PubMed]
- Foldvary-Schaefer, N., De Leon, Sanchez, I., Karafa, M., Mascha, E., Dinner, D., & Morris, H. H. (2002). Gabapentin Increases Slow-wave Sleep in Normal Adults. Epilepsia, 43(12), 1493–1497. doi:10.1046/j.1528-1157.2002.21002.x. [PubMed]
- Ebrahim, I. O., Shapiro, C. M., Williams, A. J., & Fenwick, P. B. (2013). Alcohol and Sleep I: Effects on Normal Sleep. Alcoholism: Clinical and Experimental Research, 37(4), 539`–549. doi:10.1111/acer.12006. [PubMed]
- Afaghi, A., O’Connor, H., & Chow, C. M. (2008). Acute effects of the very low carbohydrate diet on sleep indices. Nutritional Neuroscience, 11(4), 146–154. doi:10.1179/147683008×301540. [PubMed]
