Introduction
Narcolepsy is, needless to say, a disabling sleep disorder. Its effects can be incapacitating to the point of life-threatening1, depending on the severity. By medical definition, narcolepsy is characterized as extreme daytime sleepiness even with sufficient nocturnal sleep1,2. This is even more problematic when narcoleptic individuals are idle, and their sleepiness levels quickly return, ~1-2h after a daytime nap1.
Other secondary symptoms may include: sleep paralysis, hypnagogic hallucinations. As a result, a narcoleptic person is likely to struggle with sustaining daily performance. Because of the excessive daytime sleepiness, it does appear that narcoleptic patients may benefit from a polyphasic sleep schedule given their tendency to take more than 1 daily nap.
However, whether polyphasic sleep is a godsend for narcoleptics remains unclear; this post will highlight certain features in narcoleptic patients and enumerate certain recommendations.
Classification of Narcolepsy
Up to date, there are 2 notable types of narcolepsy:
- Type 1: Drastic loss of neurons that produce the orexin neuropeptide1. This narcoleptic type also goes hand in hand with cataplexy and very low levels of orexin-A in the cerebrospinal fluid.
- Type 2: Less extensive loss of orexin-producing neurons than type 1 but data is limited1. However, this type does not exhibit cataplexy and actually have normal levels of orexin-A.
Even though type 2 narcolepsy looks milder, it is also harder to diagnose; this is because other symptoms of daytime sleepiness have to be ruled out first. Regardless, narcolepsy overall has a notorious history of delayed diagnosis, including both types2,3.
- The symptoms can first manifest in children smaller than 10 years old, but peak around 15 years of age.
- In addition, there is also another secondary peak of symptoms around age of ~35 in adults2.
- Lesions in the focal central nervous system can directly alter the sleep-wake cycle and induce secondary narcoleptic symptoms4.
We know that self-diagnosis oftentimes does not reflect the true picture, but signs such as excessive daytime sleepiness are worth paying attention to. This may help you determine and get the proper consultations if you have narcoleptic symptoms early on.
The Pathological Aspects of Narcolepsy
The abnormality in sleep architecture of narcoleptic individuals is noteworthy. It is actually key to figuring out if you possess narcoleptic symptoms or not. This section will describe the pathological aspects in narcoleptics and the implications these may have for polyphasic sleeping.
Narcoleptic Napping vs Polyphasic Napping
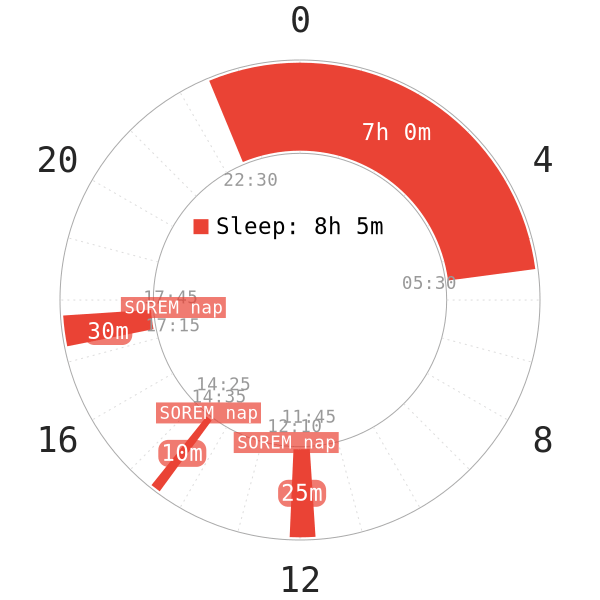
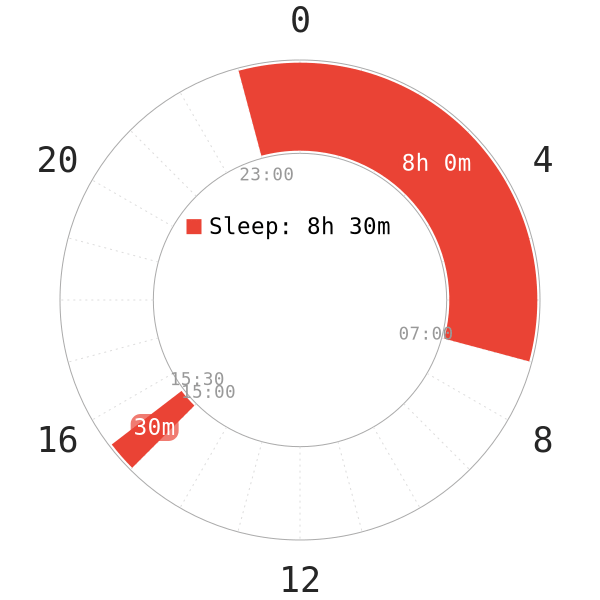
It may appear to you that polyphasic sleepers may be narcoleptic or develop narcolepsy because of reasons like “sleep deprivation“. In addition, similar to narcoleptics, polyphasic sleepers also have quick SOREM in naps. Most notably, possibly more than one daily nap can follow this SOREM tendency. After all, a core sleep at night and multiple daytime naps would make it look like an Everyman schedule, right?
While it is true that narcoleptics may involuntary practice an Everyman sleep schedule, their sleep architecture is vastly different:
- Their daytime sleepiness levels overwhelm their daytime alertness quickly. What this means is that they struggle to stay awake despite napping. Adapted polyphasic sleepers, on the other hand, do not experience such brutal alertness dips with their REM-filled naps.
- It is common that a lot of narcoleptic individuals possess increased sleep requirements and sleep duration. They can get an “adequate” amount of nocturnal sleep (7-9h), but still need to take more than one daytime nap to compensate for their weak wakeful state. Polyphasic schedules, on the contrary, reduce total sleep time to repartition REM sleep into naps.
- Narcoleptics have poor REM sleep regulation1,3. SOREM occurs soon in their nocturnal sleep, and their REM sleep behavior has abnormal timing3. Their REM can also occur in any daytime naps, regardless of hours.
- On top of all, narcoleptic individuals do not have REM sleep atonia at night3. What this means is that during REM sleep, they can perform complex behaviors such as talking, smiling and gesturing.
Polyphasic Sleep Adaptation
Depending on the severity and the symptoms you have, polyphasic sleep may still be possible. There are a few key factors to remember, however.
- If you are suffering from excessive daytime sleepiness and periods of nighttime wakefulness, establishing a strict polyphasic sleeping schedule will be very difficult. Depending on the schedule, narcolepsy may help.
- Sleeping outside the schedule will reduce or prevent adaptation to reducing schedules. If you frequently fall asleep against your will, you can try scheduling extra naps to boost alertness.
- If this doesn’t work, then polyphasic sleeping might not be possible. Note that it can take a few days or weeks to fall asleep during nap times; thus, wait for some time to see if that works. You can also talk to people in a similar situation. Regardless, a stable circadian rhythm is necessary for success.
- Because of the difficulty obtaining SWS, you should always sleep more during cores than recommended for the average adult. Instead, try extended schedules with one or even more additional core cycles. Inspect how often you struggle with nighttime wakefulness and your sleep onset duration.
- Having scheduled nap times can foster entrainment more effectively than flexible, random nap times. Performance-enhancing naps in narcoleptics can often contain SWS, due to their dysregulated sleep structure5.
Certain Benefits of Polyphasic Sleeping
- Some narcoleptics use polyphasic sleeping to deal with the tiredness and irregular sleep.
- Rather than decreasing the total sleep time, polyphasic sleep can establish a more regular schedule similar to monophasic sleep.
- Non-reducing schedules can help narcoleptics decrease the amount of sleep attacks and establish a more consistent sleep schedule. Additionally, reaching out to various support groups and asking people about their polyphasic sleeping experience is a good idea.
Note that the above information is from an interview with a narcoleptic individual. However, so far the polyphasic community has reported very little success with a fixed polyphasic schedule. Most of these attempts, though, revolve around non-reducing schedules.
Drug Consumption Warning
NOTE: If you are suffering from narcolepsy, you should be wary of attempting a polyphasic sleeping schedule. Consulting your doctor in this case. Do not attempt a polyphasic sleep schedule on medications like Xyrem or Modafinil. Modafinil is a medicine usually prescribed to people suffering from narcolepsy or hypersomnia.
- Consumption of Modafinil is not recommended due to the extremely long half life (15 hours); this means it is likely to impact the quality of multiple successive sleep sessions.
- Xyrem/sodium oxybate treats sudden muscle weakness and excessive daytime sleepiness6. It has a short half life (around 1 hour). However, it is very difficult to nap after consuming this drug. However, consult your physician if you are attempting some kind of polyphasic schedule with 1-2 daily naps.
Lifestyle warning
- If you notice that you are unable to stay awake amidst more tasks than before, do not continue with polyphasic sleep! This is very dangerous.
- Narcoleptics suffer from excessive amounts of REM, reduced SWS and possibly frequent sleep interruptions.
- Constant tiredness and attacks of falling asleep can be a dreadful combination for doing a polyphasic sleeping schedule. Cataplexy severity and frequency, however, does not have an effect on your sleep and the specific sleep needs!
- Pay close attention to your lifestyle. If your symptoms are harsh, you may have to refrain from motor tasks such as driving, unless you take a stimulant1. This is because inability to control your wakefulness can lead to accidents.
- Regarding occupations, stimulating jobs to keep you awake more easily are preferable to sedentary jobs where you can fall asleep anytime! This may be individual, so assess your condition carefully.
Main author: Crimson & GeneralNguyen
Page last updated: 8 February 2021
Reference
- Scammell, T. E. (2015). Narcolepsy. New England Journal of Medicine, 373(27), 2654–2662. doi:10.1056/nejmra1500587.
- Thorpy, M. J., & Krieger, A. C. (2014). Delayed diagnosis of narcolepsy: characterization and impact. Sleep Medicine, 15(5), 502–507. doi:10.1016/j.sleep.2014.01.015.
- Bin-Hasan, S., Videnovic, A., & Maski, K. (2018). Nocturnal REM Sleep Without Atonia Is a Diagnostic Biomarker of Pediatric Narcolepsy. Journal of Clinical Sleep Medicine, 14(02), 245–252. doi:10.5664/jcsm.6944.
- Scammell, T. E. (2003). The neurobiology, diagnosis, and treatment of narcolepsy. Annals of Neurology, 53(2), 154–166. doi:10.1002/ana.10444.
- Stampi, Claudio. Why We Nap : Evolution, Chronobiology, and Functions of Polyphasic and Ultrashort Sleep. Birkhauser, 2014.
- Mamelak, M., Black, J., Montplaisir, J., & Ristanovic, R. (2004). A Pilot Study on the Effects of Sodium Oxybate on Sleep Architecture and Daytime Alertness in Narcolepsy. Sleep, 27(7), 1327–1334. doi:10.1093/sleep/27.7.1327.
