Introduction
Melatonin was discovered in 1958 by dermatologist Aaron Lerner1. It is also known as Circadin and Slenyto by its common trade names or chemical name N-Acetyl-5-metoxytryptamine (BP)2. In addition, the human body naturally produces this hormone in a pea sized gland, located right above the center of the brain, called the pineal gland, conarium, or epiphysis cerebri3.
This chemical is responsible for sending other chemical messengers throughout the body. With this function, it coordinates specific functions that mostly regulate the sleep-wake cycle. Furthermore, the sleep-wake cycle mostly indicates the production rates and distribution of melatonin throughout the day. These processes are influenced by light and sleep. Light and dark detection with the eye retina moderates melatonin secretion. Specifically, it tends to increase during the dark period and vice versa3.
Biosynthesis of Melatonin
Melatonin is believed to exist in all living organisms including animals, plants, etc4. Nevertheless, the operating biochemical mechanism for the biosynthesis of melatonin in most animals is different than in most plants. Specifically, human melatonin biosynthesis consists of five stages5:
- First, L-tryptophan is produced in the shikimate pathway or protein catabolism.
- Via hydroxylation, L-tryptophan produces 5-hydroxy-L-tryptophan (5-HTP).
- 5-HTP’s decarboxylation produces serotonin.
- Next, serotonin converts into N-acetylseratonin.
- Finally, methylation of N-acetylseratonin forms melatonin.
Melatonin Regulation
Overall, its regulation is highly dependent on a bunch of proteins and other hormones, which light has the most effects on.
In summary, we find the following:
- In vertebrates, activation of the beta-1 adrenergic receptor by norepinephrine6 regulates melatonin secretion.
- Norepinephrine, or noradrenaline (NA), is another hormone that the body naturally produces. NA then activates specific proteins and enzymes chain reactions to induce secretion of melatonin.
- Regardless, exposure to light stops NA stimulation and destroys the proteins immediately7.
Dark Period
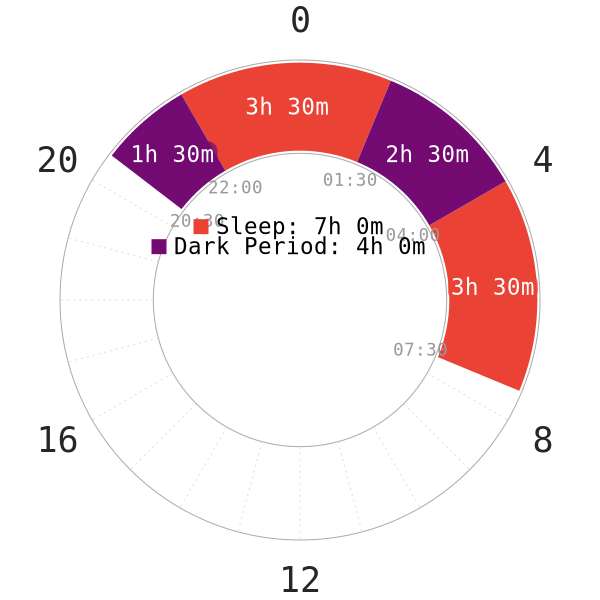
- Melatonin is important for proper SWS initiation and healthy sleep architecture8. However, exposure to blue and green light (wavelengths 400-530 nm), by 65-81%9, or roughly 2h10suppresses and delays melatonin onset.
- This feature of the rhythmic processes has been very effective in aiding the entrainment of circadian rhythms with the day-night cycle as blue light was only available during day. However, in recent years, it became increasingly apparent that this can result in circadian misalignment. Specifically, this effect worsens with exposure to artificial lighting at night.
- Some studies suggest that as little as 100 lux of room lights for 6.5 hours11, or 250 lux (office lighting) is enough to completely disrupt the melatonin levels12.
- Thus, these findings warrant minimizing all non-red light types during the dark period.
- This should not, however, compensate for the low light levels by increasing brightness of red light sources. This is because red light may have the same effect as light in the blue/green frequencies, but to a lesser extent.
- Notwithstanding, some studies have linked the misalignment of circadian processes with elevated risks of developing cardiovascular diseases13, diabetes14 and cancer15. Hence, poor sleep quality is not the only negative outcome.
Supplements
Why It is Not Good
Overall, the polyphasic community does not recommend taking melatonin supplements (MS). This is the case unless you have to rely on them, with low dose. In addition, one of the most important factors to consider before buying MS is:
- The FDA does not approve it16.
- Manmade melatonin is a dietary supplement16. Therefore, in a lot of places around the world, you can get an over-the-counter MS without any quality control (QC) or proper research17.
While most people assume MS are safe, there is a huge problem with dosage and concentration consistency in products. According to this study18, the results from analyzing 31 MS were baffling:
- “Melatonin content ranged from -83% to +478% of the labelled content.” Apparently, you DO NOT get what is labeled on the product.
- “Lot-to-lot variable within a particular product varied by as much as 465%. This variability did not appear to correlate with manufacturer or product type.” Between 20 different MS products the average lot to lot variability was +48.824% more melatonin in one batch then the other.
- “Serotonin… was identified in eight of the supplements at levels of 1 to 75 μg”, “an additional 26% were found to contain serotonin.“
“In fact, it would in most circumstances be an undesirable contaminant, as serotonin overdose can be achieved with relatively low levels and can lead to serious side effects, which in extreme cases can be fatal19.” This means that serotonin might be present in your MS, which can result in fatal serotonin overdose.
All in all, to increase the chance of getting a proper MS, look for “USP (United States Pharmacopeia) verified” MS products.
Why It is Good
For a long time, our community has received several questions about MS. There are, indeed, certain reasons why they can benefit some sleepers; whether they desire to sleep polyphasically or only improve their monophasic sleep quality is all the possible goals. Obviously, there are likely some other unique features that MS may have in conjunction with polyphasic sleep. However, much of that remains for future debate.
Overall, MS are usually useful for dealing with a few specific issues:
- This meta-analyses20 showed that MS was useful in reducing sleep onset in primary insomnia, delayed sleep phase syndrome and regulating the sleep-wake patterns in blind patients.
- As concluded by this study about jet lag21 MS was able to reduce jet leg most effectively when the passenger crossed five or more time zones particularly in the eastern direction.
- Additionally, another meta-analyses22 showed that a promising effect of MS on glycemic control.
- This sleep related meta-analysis23 showed that using MS in healthy patients reduced sleep onset by 3.9 minutes, increased sleep efficiency by 3.1% and increased sleep duration by 13.7 minutes.
- Some foods like milk and sour berries were found to contain melatonin and may improve sleep quality in humans24.
However, while melatonin has such positive traits, so far it is mostly limited to monophasic sleep.
Side Effects
So far, most studies, articles and posts made by the scientific community seem to indicate that short and long-term effects of MS are relatively safe in infants and adolescence; both low and high doses remain largely safe. However, some side effects include25-29:
- Headaches
- Dizziness
- Stomachaches
- Increased nocturnal enuresis
- Morning drowsiness
Therefore, if you have involuntarily adapted to a polyphasic schedule while also using MS, feel free to reach out and share your sleep EEG.
Author: FlexBoi
Page last updated: 13 February 2021
Reference
- Lerner, Aaron B., et al. “ISOLATION of MELATONIN, the PINEAL GLAND FACTOR THAT LIGHTENS MELANOCYTES1.” Journal of the American Chemical Society, vol. 80, no. 10, May 1958, pp. 2587–2587, 10.1021/ja01543a060. Accessed 22 Jan. 2021. [ACS]
- https://www.drugs.com/international/melatonin.html
- Soto, Lizeth. Melatonin and Its Effects: The Truth behind This Popular Supplement. [CSUTAN]
- Zhao, Dake, et al. “Melatonin Synthesis and Function: Evolutionary History in Animals and Plants.” Frontiers in Endocrinology, vol. 10, 2019, p. 249, [PubMed]
- “MetaCyc Serotonin and Melatonin Biosynthesis.” Metacyc.org [BIOCYC]
- Nesbitt, Alexander D, et al. “Headache, Drugs and Sleep.” Cephalalgia, vol. 34, no. 10, 22 July 2014, pp. 756–766, 10.1177/0333102414542662. Accessed 19 Oct. 2019. [PubMed]
- SCHOMERUS, C. “Mechanisms Regulating Melatonin Synthesis in the Mammalian Pineal Organ.” Annals of the New York Academy of Sciences, vol. 1057, no. 1, 1 Dec. 2005, pp. 372–383, 10.1196/annals.1356.028. [WILEY]
- Fourtillan, Jean B. “Role of Melatonin in the Induction and Maintenance of Sleep.” Dialogues in Clinical Neuroscience, vol. 4, no. 4, 1 Dec. 2002, pp. 395–401. [PubMed]
- Wright, Helen R., and Leon C. Lack. “EFFECT of LIGHT WAVELENGTH on SUPPRESSION and PHASE DELAY of the MELATONIN RHYTHM.” Chronobiology International, vol. 18, no. 5, Jan. 2001, pp. 801–808 [PubMed]
- Kayumov, Leonid, et al. “Blocking Low-Wavelength Light Prevents Nocturnal Melatonin Suppression with No Adverse Effect on Performance during Simulated Shift Work.” The Journal of Clinical Endocrinology & Metabolism, vol. 90, no. 5, May 2005, pp. 2755–2761 [PubMed]
- Zeitzer, Jamie M., et al. “Sensitivity of the Human Circadian Pacemaker to Nocturnal Light: Melatonin Phase Resetting and Suppression.” The Journal of Physiology, vol. 526, no. 3, Aug. 2000, pp. 695–702. [PubMed]
- Trinder, J., et al. “Inhibition of Melatonin Secretion Onset by Low Levels of Illumination.” Journal of Sleep Research, vol. 5, no. 2, 1 June 1996, pp. 77–82. [PubMed]
- Thosar, Saurabh S., et al. “Role of the Circadian System in Cardiovascular Disease.” Journal of Clinical Investigation, vol. 128, no. 6, 1 June 2018, pp. 2157–2167. [PubMed]
- Kurose, Takeshi, et al. “Circadian Rhythms and Diabetes.” Journal of Diabetes Investigation, vol. 2, no. 3, 5 June 2011, pp. 176–177. [WILEY]
- Fu, Loning, and Nicole M. Kettner. “The Circadian Clock in Cancer Development and Therapy.” Progress in Molecular Biology and Translational Science, 2013, pp. 221–282 [PubMed]
- https://www.drugs.com/melatonin.html
- What You Need To Know About Dietary Supplements. [FDA]
- Erland, Lauren A.E., and Praveen K. Saxena. “Melatonin Natural Health Products and Supplements: Presence of Serotonin and Significant Variability of Melatonin Content.” Journal of Clinical Sleep Medicine, vol. 13, no. 02, 15 Feb. 2017, pp. 275–281, jcsm.aasm.org/ViewAbstract.aspx?pid=30950&_ga=2.189656491.1066250379.1555519733-1595949527.1555429043, 10.5664/jcsm.6462. Accessed 12 Jan. 2020. [PubMed]
- Prakash, Sanjay, et al. “Mild Serotonin Syndrome: A Report of 12 Cases.” Annals of Indian Academy of Neurology, vol. 18, no. 2, 2015, p. 226, 10.4103/0972-2327.150612. Accessed 12 Feb. 2020. [PubMed]
- Auld, Fiona, et al. “Evidence for the Efficacy of Melatonin in the Treatment of Primary Adult Sleep Disorders.” Sleep Medicine Reviews, vol. 34, Aug. 2017, pp. [PubMed]
- Herxheimer, Andrew, and Keith J Petrie. “Melatonin for the Prevention and Treatment of Jet Lag.” Cochrane Database of Systematic Reviews, 22 Apr. 2002, 10.1002/14651858.cd001520. [PubMed]
- Doosti-Irani, Amin, et al. “The Effects of Melatonin Supplementation on Glycemic Control: A Systematic Review and Meta-Analysis of Randomized Controlled Trials.” Hormone and Metabolic Research = Hormon- Und Stoffwechselforschung = Hormones et Metabolisme, vol. 50, no. 11, 1 Nov. 2018, pp. 783–790, pubmed.ncbi.nlm.nih.gov/30396207/, 10.1055/a-0752-8462. Accessed 12 Feb. 2021. [PubMed]
- Brzezinski, Amnon, et al. “Effects of Exogenous Melatonin on Sleep: A Meta-Analysis.” Sleep Medicine Reviews, vol. 9, no. 1, 2005, pp. 41–50, www.ncbi.nlm.nih.gov/pubmed/15649737, 10.1016/j.smrv.2004.06.004. Accessed 31 Oct. 2019. [PubMed]
- Pereira, Nádia, et al. “Influence of Dietary Sources of Melatonin on Sleep Quality: A Review.” Journal of Food Science, vol. 85, no. 1, 19 Dec. 2019, pp. 5–13, 10.1111/1750-3841.14952. Accessed 5 Aug. 2020. [PubMed]
- Rzepka-Migut, Beata, and Justyna Paprocka. “Efficacy and Safety of Melatonin Treatment in Children with Autism Spectrum Disorder and Attention-Deficit/Hyperactivity Disorder—a Review of the Literature.” Brain Sciences, vol. 10, no. 4, 7 Apr. 2020, p. 219, 10.3390/brainsci10040219. Accessed 11 Apr. 2020. [MDPI]
- “Melatonin Side Effects: Common, Severe, Long Term.” Drugs.com, www.drugs.com/sfx/melatonin-side-effects.html.
- Andersen, Lars Peter Holst, et al. “The Safety of Melatonin in Humans.” Clinical Drug Investigation, vol. 36, no. 3, 2016, pp. 169–75, www.ncbi.nlm.nih.gov/pubmed/26692007, 10.1007/s40261-015-0368-5. [PubMed]
-
Wei, Sha, et al. “Efficacy and Safety of Melatonin for Sleep Onset Insomnia in Children and Adolescents: A Meta-Analysis of Randomized Controlled Trials.” Sleep Medicine, vol. 68, Apr. 2020, pp. 1–8, 10.1016/j.sleep.2019.02.017. Accessed 3 Apr. 2020. [PubMed]
