Introduction
There are a lot of medical conditions to be concerned about; obviously, we cannot list every possible condition and extrapolate the data with polyphasic sleeping. So far, the conditions we present in this post are unpopular in the community.
There have been people with these conditions who seek our advice, but we do not give legal medical advice for them regarding sleep. While rarer, these conditions deserve some mention at least. This will give you more opportunities to fully evaluate whether you can pursue the napping lifestyle like everyone else.
Epilepsy
Sleep deprivation is the second most common trigger for seizures; in addition, some people have it as their only trigger1. If you have epilepsy, you should not sleep deprive yourself. Non-reducing biphasic schedules would most likely be your only solution.
ADD/ADHD
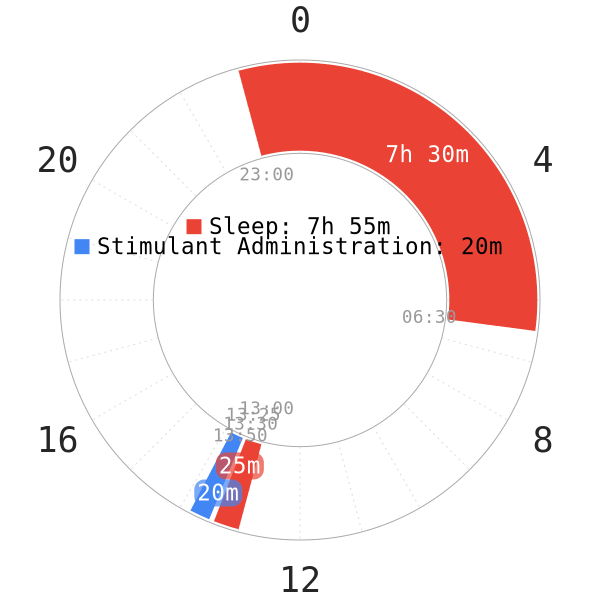
If you have a severe case of ADD or ADHD and take Adderall, methylphenidate (Ritalin), or similar medicines, polyphasic sleeping could be very difficult for you.
- Both Adderall and methylphenidate are stimulants. They are going to make falling asleep much harder unless you take small doses long before sleep.
- Fast-release Adderall has a half life of ~10 hours, while methylphenidate is ~3h. Methylphenidate is also used as a form of treatment for narcolepsy; this behavior of SOREM is similar in polyphasic sleep.
In sum, consult a physician about dosages and possibilities of polyphasic sleep while taking similar medication. Anecdotally, though, there has been certain success with napping.
- However, these successes largely limit to biphasic schedules.
- Specifically, the adapted ADHD individuals report good naps and refreshing mental state throughout the day
- On the other hand, it usually still takes them anywhere around ~10-15m to fall asleep at night. While this is a great improvement compared to their broken monophasic sleep, these sleep onset durations are usually shorter in healthy people.
Heart conditions
Sleep deprivation increases stress, which in turn increases blood pressure21. While this does not pose significant risks in healthy individuals, the risk increases in individuals with heart conditions. Thus, it should be completely avoided if you are already at high risk of getting a heart attack.
Chronic diseases
Patients with chronic diseases, like diabetes, cardiovascular diseases, sleep apnea, etc. should consult with a medical doctor. Ask them about increased health risks and medical cautions that come with the adaptation process.
For example, increased tiredness or a weakened immune system are all massive health hazards.
Depression
There appears to be a link between REM sleep frequency/quantity and depression. In particular, clinical depression appears to be a result of REM sleep alterations2. Though, it is not clear if this is the cause or symptom.
- SSRIs (common antidepressants) appear to reduce both REM quantity and also REM deprivation symptoms3. Consequently, polyphasic sleep may worsen depressive symptoms, due to REM deprivation.
- As adaptation progresses, a gradual increase in symptoms grow to be more detrimental.
- Sleep deprivation also causes mood swings, which intensifies emotions. Adapting to a polyphasic sleeping schedule will also most likely bring out loneliness; this is because polyphasic sleepers are awake during the time everyone else sleeps.
If you are suffering from depression, polyphasic sleep may still work. It can act as something to strive for, possibly getting you out of depression eventually.
- The reason why it can still work is because sleep restriction therapy has been used to treat depression4. Overall, scientists remark this method as safe, rapid and effective. Over years, it has passed the experimental developmental phases.
- Polyphasic schedules with some sleep reduction do resemble sleep deprivation therapy. Thus, anecdotally certain depressed sleepers have been able to adapt to some schedules and regain control over their sleep.
However, you should be careful about adapting to a polyphasic schedule during this time of your life. Sleep deprivation during adaptation can ultimately lead to additional stress and anxiety.
Main author: Crimson & GeneralNguyen
Last page update: 7 February 2021
Reference
- Sheps SG. Sleep deprivation: A cause of high blood pressure? Mayo Clinic . https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/expert-answers/sleep-deprivation/faq-20057959. Published April 19, 2018. Accessed October 21, 2018.
- Palagini L, Baglioni C, Ciapparelli A, Gemignani A, Riemann D. REM sleep dysregulation in depression: state of the art. Sleep Med Rev. 2013;17(5):377-390. [PubMed]
- McCarthy A, Wafford K, Shanks E, Ligocki M, Edgar DM, Dijk D-J. REM sleep homeostasis in the absence of REM sleep: Effects of antidepressants. N. 2016;108:415-425. doi:10.1016/j.neuropharm.2016.04.047. [PubMed]
- Dallaspezia, S., & Benedetti, F. (2014). Sleep Deprivation Therapy for Depression. Current Topics in Behavioral Neurosciences, 483–502. doi:10.1007/7854_2014_363. [PubMed]
