Why Reducing Sleep Schedules Require Frequent Sleep
The purpose of this page is to explore hypotheses that attempt to explain why reduced sleep schedules demand shorter wakefulness periods, or in other words, why shortened monophasic sleep does not work. The two main hypotheses are the adenosine alertness hypothesis and light sleep wakefulness sustaining hypothesis. The question can be split into two parts;
- Why a reducing monophasic sleep schedule does not work.
- Why less-TST polyphasic sleep schedules need a shorter duration between sleep episodes to work than schedules with a higher TST.
At the moment, there is more evidence for the adenosine alertness hypothesis than the light sleep wakefulness sustaining hypothesis. However, there are still uncertainties with both hypotheses; neither explains the whole situation fully.
In this article, you will learn about the evidence for each hypothesis, what they explain and otherwise.
The Adenosine Alertness Hypothesis
Adenosine Mechanisms
Crimsonflwr originally coined and explored this hypothesis. It explains why polyphasic sleepers require more sleep episodes with more sleep cut by examining the increased buildup of adenosine with prolonged wakefulness. As adenosine is the main metabolite from ATP1; the longer someone stays awake during the day, the more adenosine will build up.
- Adenosine is also the main hormone that regulates our tiredness; it has a direct relationship with the homeostatic pressure mechanism2.
- Adenosine type A1 and A2A (the specific adenosine types that are responsible for making you tired1) are present in higher concentrations in the brain.
- Additionally, during periods of prolonged wakefulness, certain chemical compounds that increase the production of adenosine (nitric oxide (NO) and prostaglandin D2) accumulate, causing adenosine to build up even faster. This in turn causes the body to release more adenosine3.
The Roles of ATP
Basically, when you are awake longer, you produce more ATP. This ATP is then metabolized to adenosine, which builds up in your brain and makes you more tired. While naps somewhat increase your alertness, they are unable to clear adenosine. This is because the clearance of adenosine increases as the slow-wave activity increases4; thus, adenosine is only cleared during SWS.
Therefore, the reason why polyphasic sleep schedules need a smaller waking period between the sleep blocks on more extreme schedules is not that light sleep provides wakefulness sustaining from naps or core(s). Rather, the buildup of adenosine makes you more tired faster after sleeping. This is because normal 20-minute naps do not clear any adenosine. Instead, short naps that are heavy on NREM2 or REM sleep will only provide a “short” amount of wakefulness, which then gets overwritten by the pre-existing concentration of adenosine when the alertness fades away.
The Unexplained Holes
There are some pieces of evidence missing to conclude for certain that this is the correct hypothesis for explaining why polyphasic sleepers need more frequent naps with lower TST schedules.
The biggest issue is that this hypothesis fails to explain:
- why morning naps need to be spaced closer to the core than later naps in the day.
- why there is a shorter wake period between naps in the morning than in the evening.
Logically, more adenosine has built up later in the day than in the evening; this may suggest that naps would need to be scheduled with a more frequent interval when there is more adenosine present. This is because naps do not clear adenosine. However, that is not what real observations show.
- In fact, people can schedule their naps with a much larger wake period in the evening than in the morning; this contradicts the conclusions of this hypothesis.
- Similarly, if this hypothesis were correct, polyphasic sleepers should only start to become very tired after up to 16 hours of wakefulness; that is the corresponding adenosine level at which monophasic sleepers start to become tired5.
Light Sleep Wakefulness Sustaining Hypothesis
This hypothesis was present in the early days of the Polyphasic Sleep Discord community. It explains why polyphasic sleepers are unable to go for long breaks without napping by concluding that light sleep is behind wakefulness sustaining.
When there is less light sleep on polyphasic sleep schedules, more frequent sleep episodes are necessary to compensate. If this hypothesis is true, it would also explain why monophasic sleepers have so much light sleep; such amounts would seem mandatory to sustain extended wake periods with only one sleep block.
The evidence for this hypothesis lies with neurotransmitter systems that are responsible for promoting wakefulness. If there are more of these hormones during NREM2, it would explain why naps reduce tiredness for only a short period of time. This is because the homeostatic pressure will appear as strong as before the nap as the levels of the hormone decreases and the somnogens remain intact.
Neurotransmitter systems that promote wakefulness
There is currently no direct connection between light sleep and any of the following hormones; however, that does not mean that there never will be in the future. This list should, therefore, only a guide to hormonal mechanics light sleep could rely on to sustain wakefulness.
These are the current known hormones/systems that are responsible for promoting wakefulness3:
- Acetylcholine
- Promotes activity typical of wakefulness and REM
- Serotonin
- Promotes a quiet waking state
- Suppresses REM sleep
- Stress response, which may play a role in why stressful people can have trouble sleeping.
- Norepinephrine
- Part of the fight-or-flight response
- Stress response
- Histamine
- Promotes wakefulness or sleep, depending on the situation.
- Orexins
- Increases wakefulness duration
- Suppresses REM sleep
- Enhances wakefulness during periods of starvation
- Neuropeptide S
- Promotes wakefulness
- Dopamine
- Very powerful wakefulness promoter
- GABA
- Some GABAergic neurons promote wakefulness, while others promote sleep.
- Glutamate
- Promotes wakefulness
There are many possibilities for how the light sleep wakefulness sustaining hypothesis could work; yet, its largest downfall is that there is very little evidence in support of it.
- The homeostatic pressure-adenosine pathway is very popular, while the effects light sleep have on wakefulness are largely unclear.
- Additionally, an increase in cortisol6 and thyroid stimulating hormone7 following sleep interruption could explain the wakefulness sustaining from short naps. This is a known phenomenon, and both of those hormones correlate with elevated alertness.
Counterpoints and critiques
- However, these alertness-inducing hormones would unlikely increase as rapidly as the alertness from a short nap. The same goes for their activity in the system for an extended period of time. For example, polyphasic sleepers are often able to stay awake for more than 6 hours during the afternoon-evening pre-core sleep gap.
There is a further critique to this hypothesis. In the Polyphasic Sleep Discord Community, two people were unable to adapt to Everyman 2 with a more than 8-hour wake period between their naps. Even after turning their first nap into a Pronap, they remain unable to do so.
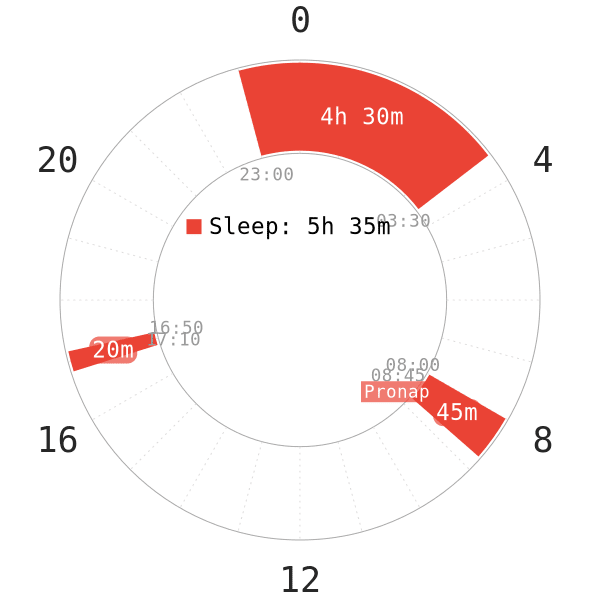
- This indicates that the extended sleep duration does not enable longer wakefulness in the wake gap right after the extended sleep.
- That said, their Pronaps contained very high proportions of REM sleep, so it does not completely discredit this hypothesis. This is because they would have possibly been able to stay awake longer if their Pronaps actually contained more light sleep.
Conclusion
When we compare these two hypotheses, evidently the adenosine alertness hypothesis has more support than the light sleep wakefulness equivalent. Even if both somewhat lack their predictive capabilities, each hypothesis would still explain why polyphasic sleepers are unable to sustain wakefulness as well as monophasic sleepers.
If there was some validity to both hypotheses, that would explain the situation to a much higher degree. This is because the hypotheses complement each other extremely well. Because of that, the real explanation is likely a combination of the two hypotheses. Regardless, as it currently stands, more evidence for light sleep and its alertness sustaining capacity would be necessary.
Main author: Crimson
Page last updated: 29 October 2021
Reference
- Bjorness, T. E., & Greene, R. W. (2009). Adenosine and sleep. Current neuropharmacology, 7(3), 238-245.
- Mantua, J., & Spencer, R. M. (2017). Exploring the nap paradox: are mid-day sleep bouts a friend or foe?. Sleep medicine, 37, 88-97. [PubMed]
- Brown, R. E., Basheer, R., McKenna, J. T., Strecker, R. E., & McCarley, R. W. (2012). Control of sleep and wakefulness. Physiological reviews. [PubMed]
- Benington, J. H., Kodali, S. K., & Heller, H. C. (1995). Stimulation of A1 adenosine receptors mimics the electroencephalographic effects of sleep deprivation. Brain research, 692(1-2), 79-85. [PubMed]
- Williamson, A. M., & Feyer, A. M. (2000). Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication. Occupational and environmental medicine, 57(10), 649-655. [PubMed]
- Stamatakis, K. A., & Punjabi, N. M. (2010). Effects of sleep fragmentation on glucose metabolism in normal subjects. Chest, 137(1), 95-101. [PubMed]
- Goichot, B., Weibel, L., Chapotot, F., Gronfier, C., Piquard, F., & Brandenberger, G. (1998). Effect of the shift of the sleep-wake cycle on three robust endocrine markers of the circadian clock. American Journal of Physiology-Endocrinology And Metabolism, 275(2), E243-E248. [PubMed]
